Elukaarevaade eluviisi ja vaimse tervise seostele vanemas eas
Vaimne tervis moodustab olulise komponendi üldisest terviseseisundist ning heaolust, mõjutades tahte- ja tegutsemisvõimet, toimetulekut igapäevaeluga ning eluga rahulolu. Vaimse tervise probleemid esinevad sagedamini noores (teisme)eas ning taas kõrgemas vanuses (WHO 2017; Laidra 2016).
Vaimse tervise häirete sagenemisel kõrgemas vanuses võivad olla erinevad põhjused. Elukaare lähenemine pakub kõige terviklikumat seletust, sidudes elus toimuva vanusspetsiifiliste muudatuste ning ajalise ja sotsiaalse dimensiooniga (Elder jt 2003). See tähendab, et teatud vanuses on tõenäolisemad mingisugused elusündmused, mis oma ajastatuse ja järjestuse kaudu mõjutavad ka vaimset tervist. Vananemine või vanemaks saamine ise ei pruugi olla kuidagi masendav protsess. Elukaare lähenemise järgi mõjutab indiviidi tervist varasemas elus kogetu – liiga palju negatiivseid, ebasoodsaid või ülejäänud ühiskonnaga võrreldes ebatüüpilisi tingimusi või sündmusi võivad kuhjudes viia halvema terviseni.
Tervist mõjutavaid elukaaremehhanisme on erinevaid (Pearlin jt 2005). Esiteks võivad elu jooksul sotsiaalsete rollide ja positsiooni omandamise viisid erineda, olenedes inimese perekonna päritolust ja lapsepõlvekodu tingimustest, aga ka naabruskonnast, kus elatakse või kus üles kasvati. Need minevikutegurid võivad tervist mõjutada vajalikule informatsioonile ja ressurssidele ligipääsu piiramise kaudu. Samuti võib raskuste pidev või korduv kogemine sellistes peamistes elusfäärides nagu perekond või tööelu mõjutada tervist negatiivselt kuhjumise kaudu. Pidev majanduslik haavatavus või korduv oht identiteedile võivad tervist mõjutada pikaajalise püsimise kaudu. Kroonilist stressi ja pingeid võib tekitada ka varane traumakogemus. Traumast tulenevad teisesed stressitekitajad ja nende traumajärgne tõenäosem kogemine võivad mõjutada vaimset tervist hilisemas eas eelkõige kaudsel teel. Samuti võib pingeid tekitada oluliste elusündmuste ajastuse ja järjestuse kõrvalekaldumine tavapärasest, mis võib mõjutada ligipääsu teatud võimalustele elus (nt haridus või tööturg). Elu tavapärase kulgemise katkestused, nagu lahkuminekud, soovimatu töökaotus või ootamatu hoolduskohustus, võivad rängemini mõjutada neid, kel pole uute olukordadega toimetulekuks piisavalt ressursse.
Elukaare lähenemine aitab selgitada ebavõrdsust tervises – elu alguses (või varemgi) haavatavust rohkem kogenud inimestel kuhjuvad sotsiaalsed ja majanduslikud riskitegurid ülejäänud elu jooksul, võimendades terviseseisundi ebavõrdsust ka hilisemas elus. Seega, lisaks inimeste endi vastutust ning isiklikke valikuid rõhutavatele ennetusmeetmetele mängivad tervise parandamises olulist rolli nii riiklikult kui ka kogukondlikult tehtavad sotsiaalsed ja majanduslikud muudatused.
Artikli eesmärk on anda ülevaade 65-aastaste ja vanemate inimeste eluviisi ja vaimse tervise seostest, selgitades vaimse tervise muutusi ning erinevusi vanema ea eluviisitegurite kaudu. Kasutame selleks SHARE (Survey on Health, Ageing and Retirement in Europe) longituuduuringu andmeid. Selle uuringuga kogutakse Euroopa riikides andmeid individuaalse vananemise, tervise ja tööturult lahkumise kohta.
Tervise vaatlemine elukaare perspektiivis võimaldab hinnata ja mõista nii eri eluetappidel kui ka eri ajastutel kogetu mõju hilisemale elule. Paljud varase elu stressi tekitavad kogemused või sündmused võivad tervisele mõju avaldada hilisemas elus.
Kui vastavaid stressitekitajaid kogetakse tundlikel või kriitilistel eluperioodidel, siis võivad need mõjutada bioloogilisi stressireguleerimise mehhanisme, närvisüsteemi või geneetilise eelsoodumuse avaldumist stressireaktsioonina (WHO 2014). Samuti võib eluviis muutuda elu erinevatel perioodidel olenevalt ümbritsevast sotsiaalsest keskkonnast ning inimese vajadustest ja võimalustest. Eluviisi aspektist vaatame lähemalt toitumist, kehalist aktiivsust, unemustreid, suitsetamist ning alkoholi tarbimist – need on peamised tegurid, mis on varasemate teadustööde põhjal olulised vaimse tervise seisukohalt.
Toitumise muutust võib vaadelda elukaare perspektiivist – esiteks kujunevad teatud toiduvaliku hoiakud ja strateegiad välja varases nooruses ning need jäävad elu jooksul üsna stabiilseks (Devine 2005). Teiseks võivad toiduga seotud valikud ja toitumiskäitumine muutuda pöördeliste elusündmuste tagajärjel, kui tekib näiteks suurem vajadus enda või oma lähedaste tervise eest hoolitseda, enesetõhusust parandada dieedivalikute kaudu või ennast toidu kaudu ümber defineerida. Kolmandaks on toiduvalikul oluline toidule omistatav tähendus ning normid, mis võivad erineda või muutuda olenevalt inimese sotsiaalsest paigutusest näiteks sotsiaalse klassi, etnilise rühma, soo või põlvkonna mõttes. Need seosed võivad toimida nii toitumisharjumuse, toidukvaliteedi mõju, erinevatele toitainetele ligipääsu kui ka toidu valmistamiseks kuluva vaba aja olemasolu kaudu. Samuti võivad toitumisharjumused erineda põlvkonniti. Näiteks 20. sajandi algupoolel sündinud inimesed kasvasid üles keskkonnas, kus oli hilisemate põlvkondadega võrreldes vähem toitumisjuhiseid või olid need teistsugused. Juhul kui põlvkonnale iseloomulikud harjumused on piisavalt levinud või vältavad piisavalt pikka aega, võivad need avalduda ka rahvastiku tervisenäitajates.
Kehalist aktiivsust võib mõista (tervise)käitumise või harjumusena – esimene neist rõhutab kognitiivset, emotsionaalset ja tegevuslikku komponenti, viimase puhul on tegu automaatse ning tihtipeale teadvustamata tegevusega (Hirvensalo ja Lintunen 2011). Elukaare perspektiivist lähtudes on leitud, et lapsepõlve ja teismeea kehaline aktiivsus ennustab ette täiskasvanuea kehalist aktiivsust, ehkki lisaks lapsepõlvetingimustele mõjutavad täiskasvanu kehalist aktiivsust ka paljud teised tegurid. See seos võib toimida motivatsiooni ja kogemuse tekkimise kaudu. Seos lapsepõlve ja vanema ea kehalise aktiivsusega on aga nõrgem – ilmselt seetõttu, et nende eluperioodide vahele jäävad pikad intervallid. Sellegipoolest võivad varasema elu kehalise aktiivsuse mustrid mõjutada ka hilisema ea kehalist aktiivsust – näiteks oskuste varajase omandamise kaudu. Samuti on uute sotsiaalsete rollide omandamise puhul tõenäolisem muutus ka kehalises aktiivsuses (Hirvensalo ja Lintunen 2011). Pensionilemineku puhul on täheldatud nii kehalise aktiivsuse vähenemist, näiteks tööle ja töölt koju liikumise arvelt, kuid samas on eelnevalt istuva loomuga töötajad selles elufaasis kehaliselt aktiivsemaks muutunud.
Uni pakub igapäevaelu probleemidele head leevendust, kuid seegi võib erineva tausta ja toimetulekustrateegiatega inimestel erineda. Üldiselt on kehvema sotsiaal-majandusliku olukorraga inimestel rohkem unehäireid – seda võivad põhjustada nii strukturaalsed ebasoodumused, nendega seotud psühholoogiline stress, eluviisitegurid kui ka
erinevad teadmised paremast unehügieenist (van de Straat jt 2020). Üldiselt esineb kesk- ja vanemaealistel naistel rohkem unehäireid kui meestel. Kui meestel on unehäired seotud vaid praeguse sotsiaal-majandusliku seisundiga, siis naiste unehäired on seotud nii praeguse kui ka lapsepõlve sotsiaal-majanduslike tingimustega. Seega, kehvemates sotsiaal-majanduslikes tingimustes üleskasvamine mõjutab vanemaealiste naiste une kvaliteeti, mida isegi hilisema elu sotsiaal-majanduslik olukord ei pruugi tasandada (van de Straat jt 2020). Samas ei tasu unustada, et unemustri muutused ja halb uni on ka vaimse tervise sage sümptom.
Suitsetamine ja alkoholi tarvitamine peegeldab stressile või pingele reageerivat käitumist, mis võib kujuneda tervist kahjustavaks üleliigse tarvitamise korral, põhjustades sõltuvust ning vaimse tervise probleeme. Üldiselt on vanemaealise rahvastiku puhul tervist kahjustav tubaka- ja alkoholitarvitamine olnud levinum meeste seas, mõjutades nende haigestumust ja suremust enam. Kuna meeste eluiga on Eestis oluliselt lühem naiste elueast, siis ei pruugi see mõju tervisetulemitele aga uuringute põhjal välja tulla, sest vastajate seas on pigem tervemad ning kauem elus püsinud inimesed.
Meie analüüsis on Eesti SHARE uuringu 2013. aasta andmed, mil küsiti põhjalikumalt lapsepõlvetingimuste kohta – see võimaldab erinevaid elukaare tingimusi arvesse võtta. Aluseks on 2011. aastal intervjueeritud 65-aastased ja vanemad inimesed, kes vastasid ka 2013. aastal. Analüüsisime vastanute vaimse tervise muutust 2013. aastaks. Eesti lõppvalimi suurus 65-aastaste ja vanemate inimestega on 2026 inimest (684 meest ja 1342 naist).
Peamiselt vaatleme EURO-D depressiivse meeleolu skaalat, mis on rahvusvaheliselt välja töötatud, võrreldav ja valideeritud just kesk- ja vanemaealise rahvastiku jaoks (Guerra jt 2015). See skaala mõõdab 12 erineva sümptomi (sh alanenud meeleolu, enesetapumõtted, süütunne, ärrituvus, üksindustunne, unehäired, huvi puudumine, söömishäired, väsimus, keskendumisvõime langus, nutmishood, naudingu puudus) olemasolu viimase nelja nädala jooksul, mis on kokku liidetud koondskooriks – suurem väärtus viitab depressiivsuse esinemisele (juhul kui skoori väärtus on rohkem kui 3). Tegemist pole meditsiiniliselt diagnoositud depressiooni tulemiga, vaid enesehinnanguliste vastustega, mille tõttu on depressiivsuse levimus oluliselt suurem depressiooni levimusest, kuid aitab see-eest hinnata inimeste hulka, kes vajaksid mingit sorti vaimse tervise (esma)abi. Käesoleva artikli puhul saab seetõttu rääkida korrektsemalt „depressiivsusest“ või „depressiivsuse sümptomitest“.
Üldiselt on Eesti keskmine depressiivsuse sümptomite arv 65-aastaste ja vanemate seas võrreldes teiste uuringus osalenud riikide omaga suhteliselt suur. Eesti vastajatel oli depressiivsuse levimus 2011. aastal 40% (naistel 46%, meestel 29%), 2013. aastaks oli see mõnevõrra kahanenud 38%ni (naistel 43%ni ning meestel 28%ni).
Kuigi naistel on nii Eestis kui ka teistes riikides meestest suurem depressiivsuse sümptomite arv, on Eesti meeste suhteline positsioon halvem kui naistel Euroopa võrdluses (joonis 2.4.1). Eesti meestel on keskmiselt 2,5 depressiivsuse sümptomit ning see on üks kõrgemaid näitajaid 2013. aastal – sarnased on veel vaid Itaalia, Prantsusmaa ja Sloveenia mehed. Eesti naistel on aga keskmiselt 3,4 sümptomit (ületades depressiivsuse lävendi) – see on veidi madalam kui Hispaanias ja Itaalias ning on võrreldav Prantsusmaa naistega.
J2.4.1.R
maiko.koort
2023-02-06
library(ggplot2)
library(tidyr)
library(scales)
#faili sisselugemine ja andmete formaadi korrigeerimine
J241=read.csv2("PT2-T2.4-J2.4.1.csv",header=TRUE, encoding ="UTF-8")
J241$Keskmine=as.numeric(J241$Keskmine)
J241$Usaldusintervallid=as.numeric(J241$Usaldusintervallid)
J241$Usaldusintervallid.1=as.numeric(J241$Usaldusintervallid.1)
J241$Riik=as.factor(J241$Riik)
J241$Riik=factor(J241$Riik,levels=rev(levels(J241$Riik)))
#joonis
ggplot(J241,aes(x=Riik,y=Keskmine,col=Sugu))+
geom_point(cex=3)+
geom_errorbar(aes(x=Riik,ymin=Usaldusintervallid,ymax=Usaldusintervallid.1),width=0.1,linewidth=0.9)+
theme_minimal()+
coord_flip()+
scale_y_continuous(limits=c(1,5))+
scale_color_manual(values=c("#6666cc","#FF3600"))+
theme(text = element_text(color="#668080"),axis.text=element_text(color="#668080",face=c(1,1,1,1,1,1,1,1,1,2,1,1)),legend.title=element_blank())+
ylab("Keskmine depressiivsus (EURO-D)")## Warning: Vectorized input to `element_text()` is not officially supported.
## ℹ Results may be unexpected or may change in future versions of ggplot2.Vanusega kasvab keskmine depressiivsuse sümptomite arv kõigis uuringus osalenud riikides. Samas ei ilmne 85-aastaste ja vanemate meeste puhul sümptomite arvus riikide vahel olulisi erinevusi. Depressiivsuse olemasolu lävendi ehk keskmiselt kolme sümptomi taseme ületavad Eesti naised juba 60. eluaastate keskel, samas kui mehed jõuavad sama kõrge näitajani alles 80. eluaastateks (joonis 2.4.2).
J2.4.2.R
maiko.koort
2023-02-06
library(ggplot2)
library(tidyr)
library(scales)
#faili sisselugemine ja andmete formaadi korrigeerimine
J242=read.csv2("PT2-T2.4-J2.4.2.csv",header=TRUE, encoding ="UTF-8")
J242$Keskmine=as.numeric(J242$Keskmine)
J242$Usaldusintervallid=as.numeric(J242$Usaldusintervallid)
J242$Usaldusintervallid.1=as.numeric(J242$Usaldusintervallid.1)
names(J242)[1]="Sünniaasta"
#joonis
ggplot(J242,aes(x=Sünniaasta,y=Keskmine,col=Sugu))+
geom_point(position=position_dodge(0.2),cex=3)+
geom_errorbar(aes(x=Sünniaasta,ymin=Usaldusintervallid,ymax=Usaldusintervallid.1),width=0.2,linewidth=0.9,position=position_dodge(0.2))+
theme_minimal()+
scale_color_manual(values=c("#6666cc","#FF3600"))+
theme(text = element_text(color="#668080"),axis.text=element_text(color="#668080"),legend.title=element_blank())+
ylab("Keskmine depressiivsus (EURO-D)")Peamiste eluviisi kirjeldavate tunnustena vaatleme erinevate toitainete tarvitamissagedust, mõõduka ja intensiivse kehalise aktiivsuse sagedust, unehäirete olemasolu, suitsetamist (kas suitsetab praegu või on varem suitsetanud) ning suures koguses alkoholi tarvitamise sagedust. Peamised sotsiaal-demograafilised tunnused, millele tulemusi regressioonimudelites kohandame, on vanus, sünniaasta, sünniriik (Eestis või välismaal sündinud), elukoht (maa või linn), perekonnaseis (abielus/kooselus, lahutatud / lahku läinud, vallaline, lesk), laste arv, hariduses osaletud aastate arv ning tööhõiveseisund (kodune/haige, pensionil, töötav). Tervist kirjeldavad eelnev depressiivsus (EURO-D 2011. aastal), tervisest tingitud tegevuspiirangute tase (tõsised, mõõdukad, pole piiranguid) ning kehamassiindeks – kõigile neile tunnustele on mudelid kohandatud. Lapsepõlvekodu tingimuste kohandamiseks kasutatakse kolme tunnust, mis kirjeldavad lapsepõlves kogetud elamistingimusi (lapsepõlvekodu tihelioleku aste ehk tubade arv inimeste kohta), majanduslikke tingimusi (lapsepõlve pere majandusliku toimetuleku hinnang) ning terviseseisundit (lapsepõlve tervise enesehinnang).
Kõikidele tunnustele kohandatud lõplike regressioonimudelite tulemused eluviisi ja vaimse tervise seoste kohta meestel ja naistel on näidatud joonisel 2.4.3. Nende põhjal on näha, et kuigi üldiselt on seosed vähesed või nõrgapoolsed, esineb depressiivsus oluliselt sagedamini neil naistel ja meestel, kes kogevad unehäireid ning kelle puhul ei ole teada alkoholitarvitamise sagedust või kes tarvitavad seda harva (1–3 korda kuus võrreldes viimasel kolmel kuul mitte kordagi tarvitanutega). Kuna unehäired on üks depressiivsuse peamisi sümptomeid, siis on tulemus ootuspärane – meie analüüsis kohandatud tunnused seda seost ära ei kaota. Alkoholitarvitamise tulemused võivad tunduda esialgu paradoksaalsena. Tulemust aga selgitab asjaolu, et alkoholi harva või üldse mitte tarvitavate seas on rohkem krooniliste haiguste või tegevuspiirangutega inimesi, seega olemasolev halb tervise seisund on nii alkoholi mittetarvitamise kui ka halvema vaimse tervise taga (Abuladze jt 2020).
Naiste puhul seletavad sotsiaal-demograafilised ja -majanduslikud tunnused (v.a perekonnaseis ja laste arv) depressiivsuse erinevusi unehäirete, alkoholi tarvitamise ning mõõduka kehalise aktiivsuse puhul mõnevõrra, tervisetunnused aga seletavad erinevusi kõige enam (tabel 2.4.1). Mõõduka kehalise aktiivsuse puhul isegi nii palju, et olulised erinevused depressiivsuse šansis kaovad (mudel 6, tabel 2.4.1). Lapsepõlveteguritest seletavad depressiivsuse erinevusi mõnevõrra lapsepõlve majanduslikud tingimused ning lapsepõlve tervise enesehinnang.
Meestel on depressiivsuse šanss kaks korda suurem neil, kes sõid valgurikkaid toite harvem kui kolmel päeval nädalas võrreldes igapäevaste sööjatega (tabel 2.4.2). Peale tervisetunnustele kohandamist kadus tunnuse olulisus, viidates sellele, et terviseprobleemid võivad mõjutada vastavate toitainete tarbimissagedust (mudel 6, tabel 2.4.2). Kuid lapsepõlvetingimustele kohandades muutus see tunnus taas oluliseks, viidates siiski teatud kahjuliku seose olemasolule toitainete tarbimises (mudelid 8 ja 9, tabel 2.4.2).
Ehkki depressiivsuse šansi erinevusi seletab terviseseisund nii meestel kui ka naistel kõige rohkem, paistab ühe erinevusena välja, et lapsepõlvetingimustele kohandamine vähendab depressiivsuse tekke erinevusi mõnevõrra just naiste seas. Lapsepõlvetingimused, eelkõige majanduslik olukord ja tervise enesehinnang, selgitavad vaimse tervise erinevusi naistel. Seega võib öelda, et naiste seas on lapsepõlves kogetud ebavõrdsus kandunud hilisemasse ellu, võimendades teatud määral eluviisi negatiivseid seoseid vaimsele tervisele vanemas eas.
Niisiis ennustavad Eesti vanemaealiste depressiivsust kõige selgemini unehäirete olemasolu ning alkoholitarvitamise sageduse erinevused nii meeste kui ka naiste puhul. Meestel aga on märgata ka valgurikka toitumise olulist rolli depressiivsuse tekkes. Ülejäänud eluviisi tegurid, nagu erinevate toitainete tarbimine, kehaline aktiivsus ja suitsetamine, depressiivsust vanemas eas hästi ei ennusta.
J2.4.3.R
maiko.koort
2023-02-14
library(ggplot2)
library(tidyr)
library(scales)
#faili sisselugemine ja andmete formaadi korrigeerimine
J243=read.csv2("PT2-T2.4-J2.4.3.csv",header=TRUE, encoding ="UTF-8")
J243$OR=as.numeric(J243$OR)
J243$Tunnus=sub("_"," ",J243$Tunnus)
J243$Tunnus=sub("_"," ",J243$Tunnus)
J243$Väärtus=sub("_"," ",J243$Väärtus)
J243$Väärtus=sub("_"," ",J243$Väärtus)
J243$usaldusintervall=as.numeric(J243$usaldusintervall)
J243$usaldusintervall.1=as.numeric(J243$usaldusintervall.1)
J243$Väärtus=as.factor(J243$Väärtus)
J243$Tunnus=as.factor(J243$Tunnus)
J243$Tunnus=factor(J243$Tunnus,levels(J243$Tunnus)[order(c(9,5,4,3,6,2,8,7,1))])
J243$Väärtus=factor(J243$Väärtus,levels(J243$Väärtus)[order(c(2,3,1,11,5,6,7,8,9,12,4,10))])
J243$Sugu="Mehed"
J244=read.csv2("PT2-T2.4-J2.4.4.csv",header=TRUE, encoding ="UTF-8")
J244$OR=as.numeric(J244$OR)
J244$usaldusintervall=as.numeric(J244$usaldusintervall)
J244$usaldusintervall.1=as.numeric(J244$usaldusintervall.1)
J244$Väärtus=as.factor(J244$Väärtus)
J244$Tunnus=as.factor(J244$Tunnus)
J244$Tunnus=factor(J244$Tunnus,levels(J244$Tunnus)[order(c(9,5,4,3,6,2,8,7,1))])
J244$Väärtus=factor(J244$Väärtus,levels(J244$Väärtus)[order(c(2,3,1,11,5,6,7,8,9,12,4,10))])
J244$Sugu="Naised"
J243=rbind(J243,J244)
J243$OR=as.numeric(J243$OR)
#joonis
ggplot(J243)+
theme_minimal()+
geom_abline(aes(slope=0,intercept=1),linetype="dashed")+
geom_errorbar(aes(x=Väärtus,ymin=usaldusintervall,ymax=usaldusintervall.1,col=Sugu),width=0.2)+
geom_point(aes(x=Väärtus,y=OR,col=Sugu),cex=2)+
scale_color_manual(values=c("#6666cc","#FF3600"))+
theme(text = element_text(color="#668080"),axis.text=element_text(color="#668080"))+
facet_grid(Tunnus~Sugu,scales="free_y", space="free",labeller = label_wrap_gen(5))+
theme(legend.position = "none")+
coord_flip()+
xlab("")+
ylab("Šansisuhe (OR)")+
theme(strip.text.y = element_text(angle = 360,color="#668080"),strip.text.x = element_text(face = "bold",size=10,color="#668080"))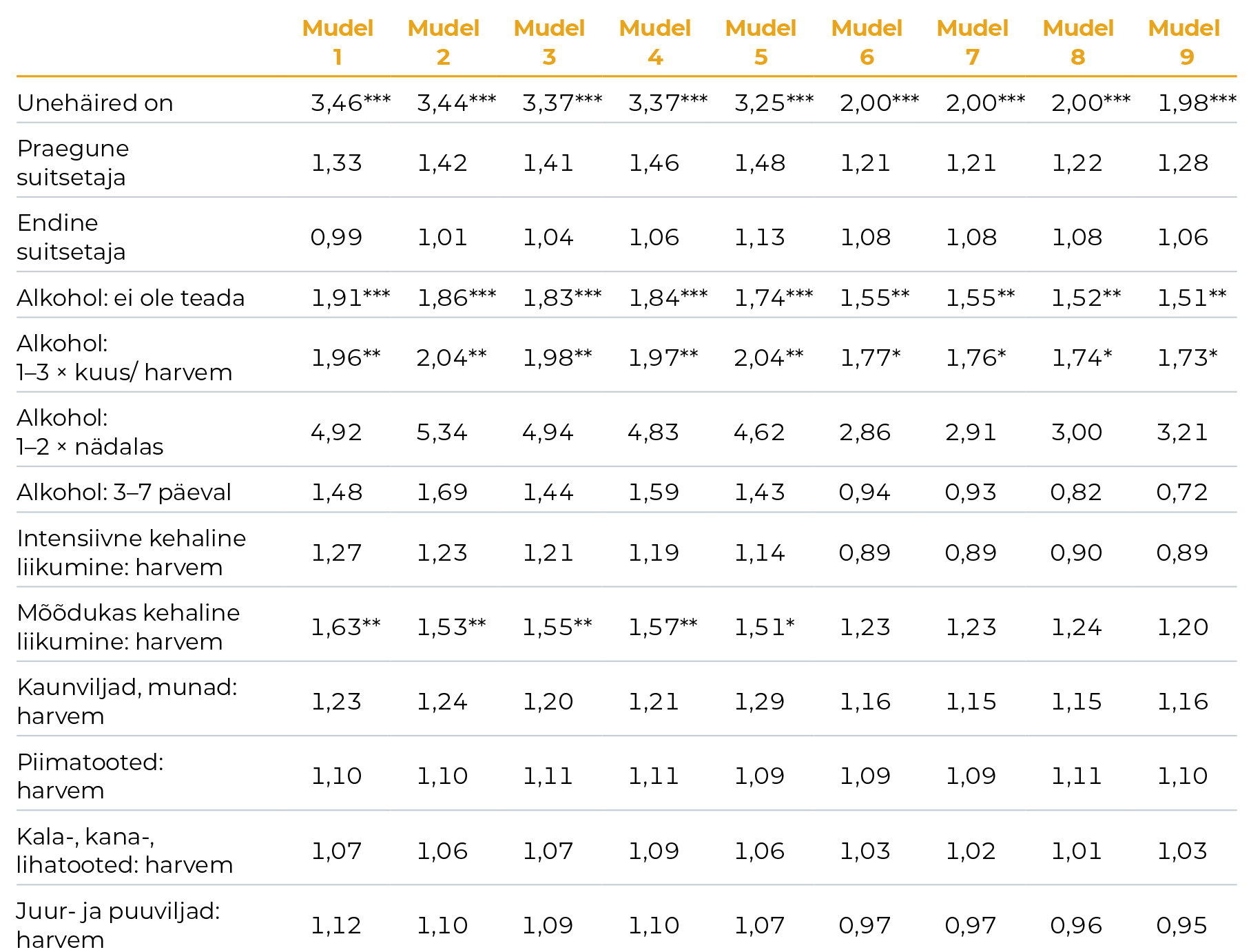
Võrdlusrühmad: unehäireid ei ole; pole kunagi suitsetanud; pole 3 kuu jooksul alkoholi tarvitanud; igapäevane intensiivne kehaline tegevus; igapäevane mõõdukas kehaline tegevus; igapäevane kaunviljade, munade, piimatoodete, kala-, kana-, lihatoodete ning juur- ja puuviljade tarbimine.
Tunnustele kohandamise järjekord mudelites: mudel 1: eluviisi tunnused; mudel 2: + vanus, sünnikohort; mudel 3: + päritolu, elukoht; mudel 4: + pereseis, laste arv; mudel 5: + haridus, hõiveseisund: mudel 6: + depressiivsus, tegevuspiirangud, KMI; mudel 7: + lapsepõlvekodu tihelioleku aste; mudel 8: + lapsepõlve majanduslik seis; mudel 9: + lapsepõlve terviseseisund.
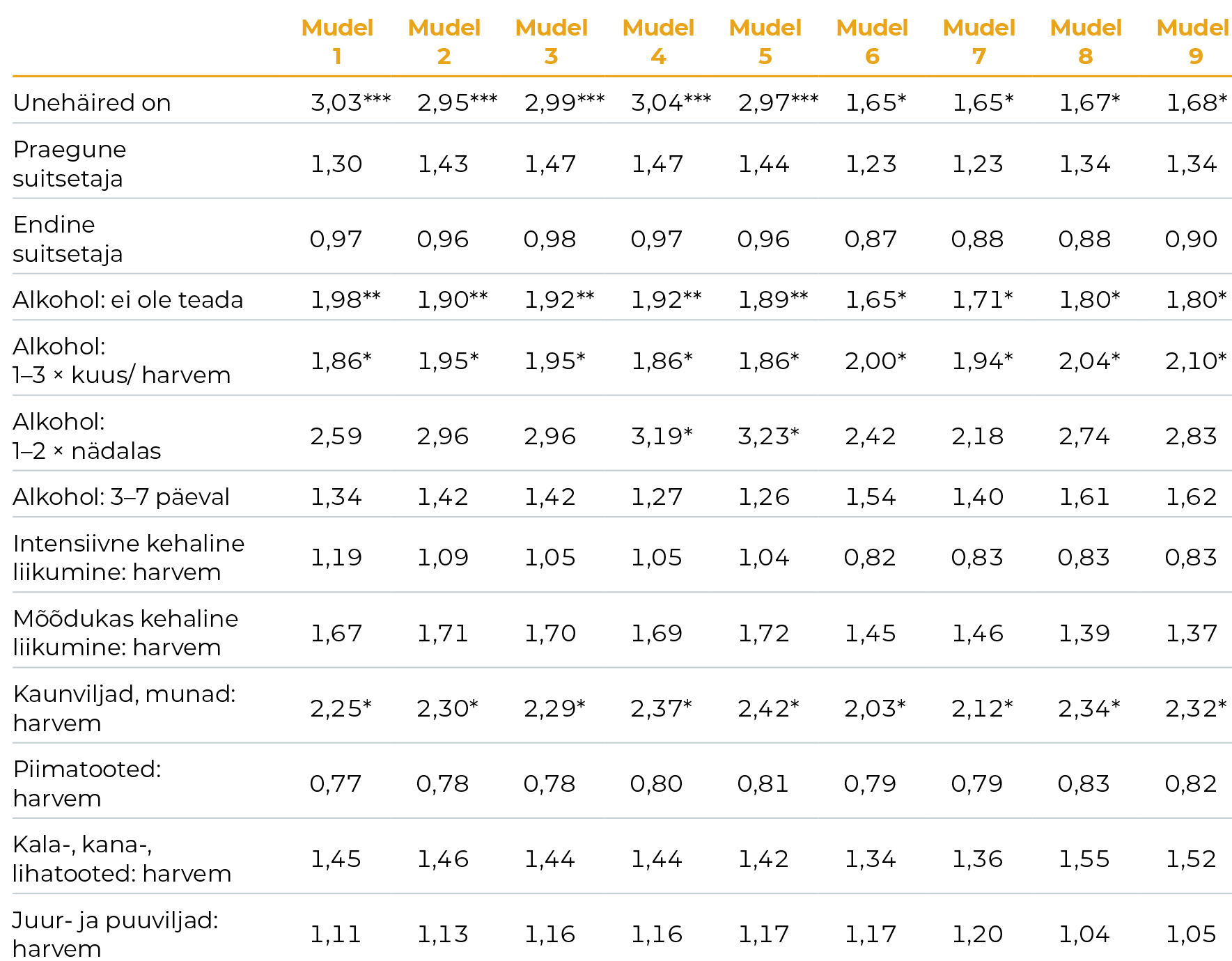
Märkused:
Statistiline olulisus: *** p < 0,001; ** p < 0,01; *p < 0,05; p >= 0,05p
Võrdlusrühmad: unehäireid ei ole; pole kunagi suitsetanud; pole 3 kuu jooksul alkoholi tarvitanud; igapäevane intensiivne kehaline tegevus; igapäevane mõõdukas kehaline tegevus; igapäevane kaunviljade, munade, piimatoodete, kala-, kana-, lihatoodete ning juur- ja puuviljade tarbimine.
Tunnustele kohandamise järjekord mudelites: mudel 1: eluviisi tunnused; mudel 2: + vanus, sünnikohort; mudel 3: + päritolu, elukoht; mudel 4: + pereseis, laste arv; mudel 5: + haridus, hõiveseisund: mudel 6: + depressiivsus, tegevuspiirangud, KMI; mudel 7: + lapsepõlvekodu tihelioleku aste; mudel 8: + lapsepõlve majanduslik seis; mudel 9: + lapsepõlve terviseseisund.
Kokkuvõte
Enesehinnangulise mõõdiku järgi oli 2013. aastal Eesti 65-aastaste ja vanemate inimeste seas keskmine depressiivsuse sümptomite arv Euroopa võrdluses suhteliselt suur. Suhteline positsioon võrreldes teiste riikidega oli meestel halvem kui naistel, ehkki keskmine depressiivsuse sümptomite arv oli suurem naistel. Veel vanemas eas – 85-aastaste ja vanemate puhul – aga olid mehed kõikides riikides sarnaselt depressiivsed, viidates meeste puhul universaalsemate depressiivsuse tegurite mõjule selles eas. Nii nagu depressiivsus on üldiselt levinum pigem naiste kui meeste seas, arenes tõsine depressiivsuse seisund naistel varem kui meestel – depressiivsuse olemasolu lävendi piiri ületasid Eesti naised juba 60. eluaastates, mehed aga alles 80. eluaastates.
Kõikidele tunnustele kohandamise järel oli Eesti 65-aastaste ja vanemate meeste ja naiste depressiivsuse tekke šanss oluliselt suurem unehäiretega inimestel ning neil, kes tarvitasid alkoholi harva (võrreldes mittetarvitanutega). Unehäirete seos vaimse tervisega on teada ka varasemast – see on üks peamisi depressiooni ja depressiivsuse sümptomeid, kuid käesolev analüüs viitas sellele, et vanemaealiste unehäirete seos depressiivsusega on seletatav eelkõige tervisest tingitud tegevuspiirangutega ning eelnevalt esinenud depressiivsuse sümptomitega. Tegevuspiirangute oluline roll on kooskõlas teoreetilise raamistikuga, mille järgi ei ole ühiskondlik korraldus (nii sotsiaalne kui ka institutsionaalne) inimeste tervisest tingitud vajadustele järele tulnud (Verbrugge ja Jette 1994). Eelneva depressiivsuse oluline roll aga viitas vaimse tervise probleemide püsimisele, mida tervishoiusektor ega inimese sotsiaalne keskkond pole suutnud ennetada.
Seega võiksid vaimse tervise parandamise viisid vanemaealiste puhul põhineda komplekssel ja terviklikul lähenemisel, võttes arvesse nii sotsiaalse kui ka füüsilise keskkonna ning üldise heaolu kujundamise vajadust.
Alkoholi mitte tarvitavad vanemaealised inimesed on tihti juba eksisteerivate terviseprobleemidega; alkoholi tarvitavad aga on tervemad nii füüsilise kui ka vaimse tervise poolest (Abuladze jt 2020). Naistel selgitasid tervisetegurid ka depressiivsuse erinevusi mõõduka kehalise aktiivsuse puhul. Erinevalt võib-olla teistest elufaasidest või levinud soovitustest leidsime, et kehaline aktiivsus vanemas eas sõltus väga palju olemasolevast terviseseisundist. Erinevad haigused või terviseprobleemid piiravad igapäevatoimetusi, ühiskonnaelus osalemist ning vaimse tervise säilitamist.
Seega, kui vältida ühiskonna tasandil sotsiaalseid ja füüsilisi barjääre, mis takistavad erineva terviseseisundiga inimestel elus osalemist (Verbrugge ja Jette 1994), siis võiks kehalise aktiivsuse positiivseid mõjusid depressiivsuse leevendamisele või vastavate sümptomite ärahoidmisele näha ka Eesti vanemate naiste puhul.
Ka meestel selgitasid käesoleva terviseseisundi tunnused erinevusi depressiivsuses, aga eelkõige üldise toitumise kvaliteedi kaudu. Seega ka toitumisvalikute mõju depressiivsuse tekkele toimis hiljuti kogetud tegevuspiirangute ning eelneva depressiivsuse kogemuse kaudu – nende terviseprobleemide olemasolul jätsid mehed teatud toitainete söömise unarusse, mis võis omakorda mõjuda vaimsele tervisele halvasti. Huvitav oli aga see, et erinevalt naistest ei seleta lapsepõlvetingimused meeste depressiivsuse tekke ebavõrdsusi hilisemas eas.
Elukaare varasematel etappidel kogetu omas teatud seoseid vaimse tervisega vanemas eas, ehkki hiljutine või käesolev terviseseisund mõjutas vaimse tervisega seotud eluviisi tegureid kõige tugevamalt. Lapsepõlve sotsiaal-majandusliku ning terviseolukorra negatiivset seost hilisema elu unehäiretega ning seeläbi ka vaimse tervisega puhverdasid mõnevõrra vanema ea sotsiaal-majanduslikud tingimused, kuid mitte tervenisti, nii et lapsepõlves kogetud ebavõrdsuse seos tervisega kandus üle ka elukaare viimastesse aastakümnetesse. Seda oli märgata selgelt naiste puhul, mis kinnitas ka varasemaid tulemusi (van de Straat jt 2020).
Ehkki lapsepõlves võivad olla omandatud ka tervist toetavad harjumused või suhtumised seoses toitumise või kehalise aktiivsusega (Hirvensalo ja Lintunen 2011; Devine 2005), see seos Eesti vanemaealiste puhul selgelt esile ei tulnud. Vastupidi – kui hiljutiste tervisest tulenevate tegevuspiirangute ja vaimse tervise probleemidega tegeledes parandada naiste kehalist aktiivsust ja meeste toitumist, võiks see omakorda vähendada vanema ea depressiivsust.
Kui eemaldada sotsiaalsed ja füüsilised barjäärid ühiskonnas osalemiselt, ennetada ja leevendada vanemaealiste depressiivsuse sümptomeid õigeaegselt ning parandada ka tulevaste põlvkondade lapsepõlvetingimusi, paraneksid
vaimse tervise tulemid vanemas eas. Ehkki vanemas eas on depressiivsuse sümptomite levimus taas suurem kui eelnevatel elukümnenditel, peaks nende leevendamisel ja ennetamisel Eestis rohkem arvesse võtma vanemaealiste sotsiaal-majanduslikku ja tervisest tulenevat ebavõrdsust. See tähendab, et vaimse tervise järelevalve ning terviseteenuste pakkumine võiks rohkem arvestada erinevate sünnipõlvkondade tausta, aga ka selgemalt sihitama haavatavama elukäiguga inimesi.
Abuladze, L., Opikova, G., Lang, K. (2020). Factors associated with incidence of depressiveness among the middle-aged and older Estonian population. SAGE Open Medicine, 8, 1−12. DOI: 10.1177/2050312120974167.
Devine, C. J. (2005). A Life Course Perspective: Understanding Food Choices in Time, Social Location, and History. Journal of Nutrition Education and Behavior, Vol. 37(3), 121–128. https://doi.org/10.1016/S1499-4046(06)60266-2.
Elder, G. H., Johnson, M. K., Crosnoe, R. (2003). The emergence and development of life course theory. In Handbook of the life course (pp. 3-19). Springer, Boston, MA.
Guerra, M., Ferri, C., Llibre, J., Prina, A. M., Prince, M. (2015). Psychometric properties of EURO-D, a geriatric depression scale: A cross-cultural validation study. BMC Psychiatry, 15(1). doi:10.1186/s12888-015-0390-4
Hirvensalo, M., Lintunen, T. (2011). Life-course perspective for physical activity and sports participation. Eur Rev Aging Phys Act 8, 13–22. https://doi.org/10.1007/s11556-010-0076-3.
Laidra K. (2016). Vaimne ja kognitiivne tervis. In: Sakkeus L, Leppik L. Pilk hallile alale. SHARE Eesti uuringu esimene ülevaade ja soovitused eakate poliitika kujundamiseks. Tallinn: Tallinna Ülikool, 73–96.
Pearlin, L. I., Schieman, S., Fazio, E. M, Meersma, S. C. (2005). Stress, Health, and the Life Course: Some Conceptual Perspectives. Journal of Health and Social Behavior, 46 (June): 205–219.
van de Straat, V., Cheval, B., Schmidt, R. E., Sieber, S., Courvoisier, D., Kliegel, M., Burton-Jeangros, C., Cullati, S., Bracke, P. (2020). Early predictors of impaired sleep: a study on life course socioeconomic conditions and sleeping problems in older adults. Aging & Mental Health, 24:2, 322–332, DOI: 10.1080/13607863.2018.1534078.
Verbrugge, L. M., Jette, A. M. (1994). The disablement process. Social Science and Medicine, 38(1), l-14.
WHO (2014). World Health Organization and Calouste Gulbenkian Foundation. Social determinants of mental health. Geneva, World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/112828/9789?sequence=1.
WHO (2017). World Health Organisation. Mental health of older adults: fact sheet. http://www.who.int/mediacentre/factsheets/fs381/en/.